What Is an Imaging Trial? Complete Guide to Medical Research Imaging
.png?width=2000&height=1360&name=pic%20(1).png)
An imaging trial is a research study conducted with volunteers to evaluate the effectiveness of imaging procedures in detecting, diagnosing, guiding, or monitoring the treatment of diseases. Unlike traditional clinical trials that focus primarily on testing drugs or treatments, imaging trials specifically assess imaging technologies and their applications in healthcare.
What is an Imaging Trial: The Basics
Imaging trials are essential components of medical research that help advance our understanding of diseases and improve patient care through better diagnostic and monitoring tools. These specialized studies evaluate how well imaging techniques can detect, measure, or track changes in the body.
According to the National Cancer Institute's Cancer Imaging Program:
"An imaging clinical trial is a research study conducted with people who volunteer to take part. Each study answers specific scientific questions."
These trials differ from standard clinical practice imaging in several key ways. While clinical practice focuses on individual patient diagnosis and care, imaging trials aim to generate standardized, quantifiable data that can be analyzed across groups of participants.
Types of Imaging Trials:
- Diagnostic imaging trials - Evaluate how well imaging techniques can detect or diagnose specific conditions
- Monitoring imaging trials - Assess imaging methods for tracking disease progression or treatment response
- Comparative imaging trials - Compare different imaging modalities for specific applications
- Virtual imaging trials - Use computer simulations to evaluate imaging technologies without human subjects
The Purpose and Importance of Imaging Trials
Imaging trials serve multiple crucial purposes in advancing medical science and patient care. They help researchers determine which imaging techniques are most effective for specific conditions, establish standardized protocols, and develop new approaches to visualizing disease.
Key Objectives of Imaging Trials
- Evaluate the accuracy and reliability of imaging techniques
- Develop new imaging biomarkers for disease detection and monitoring
- Assess the safety of imaging procedures
- Compare the effectiveness of different imaging modalities
- Establish standardized imaging protocols for clinical use
In oncology, imaging trials are particularly valuable. As noted in a study published in the PMC:
"Imaging techniques are increasingly used in oncological clinical trials to provide evidence for decision making."
These trials help determine which imaging approaches can best detect tumors, monitor treatment response, and predict patient outcomes.
Also Read: Clinical Trial Phases: Complete Guide to All 4 Stages (2025)
How Imaging Trials Differ from Traditional Clinical Trials
While traditional clinical trials focus on testing treatments or interventions, imaging trials have distinct characteristics that set them apart:
Key Differences:
| Aspect | Traditional Clinical Trials | Imaging Trials |
|---|---|---|
| Primary Focus | Testing treatments or interventions | Evaluating imaging technologies |
| Endpoints | Clinical outcomes (survival, symptoms) | Imaging metrics (sensitivity, specificity) |
| Participant Experience | May involve treatment administration | Primarily involves imaging procedures |
| Data Collection | Clinical measurements, lab tests | Images and image analysis |
According to Lars Johansson, Chief Scientific Officer at Imaging CRO Antaros Medical:
"In clinical practice, imaging is used primarily by healthcare professionals for diagnosis and follow-up of disease progression/regression. That is, to detect a disease or stage its severity."
In contrast:
"In clinical trials for drug development, imaging serves to quantify treatment effect in a standardised way that allows for comparisons."
This fundamental difference in purpose shapes how imaging trials are designed, conducted, and analyzed.
The Process of an Imaging Trial
Imaging trials follow a structured process to ensure scientific validity and participant safety. Understanding this process can help potential volunteers know what to expect.
1. Study Design and Protocol Development
Before an imaging trial begins, researchers develop a detailed protocol that outlines:
- The specific imaging techniques to be used
- Participant eligibility criteria
- Data collection methods
- Analysis approaches
- Quality control measures
2. Participant Recruitment and Screening
Volunteers are recruited based on specific criteria relevant to the study's objectives. This may include people with certain medical conditions or healthy volunteers for comparison.
3. Informed Consent
All participants must provide informed consent after being fully informed about:
- The purpose of the study
- Required procedures
- Potential risks and benefits
- Rights as a research participant
4. Image Acquisition
Participants undergo the specified imaging procedures according to standardized protocols. This might involve:
- MRI (Magnetic Resonance Imaging)
- CT (Computed Tomography)
- PET (Positron Emission Tomography)
- Ultrasound
- X-ray or other imaging modalities
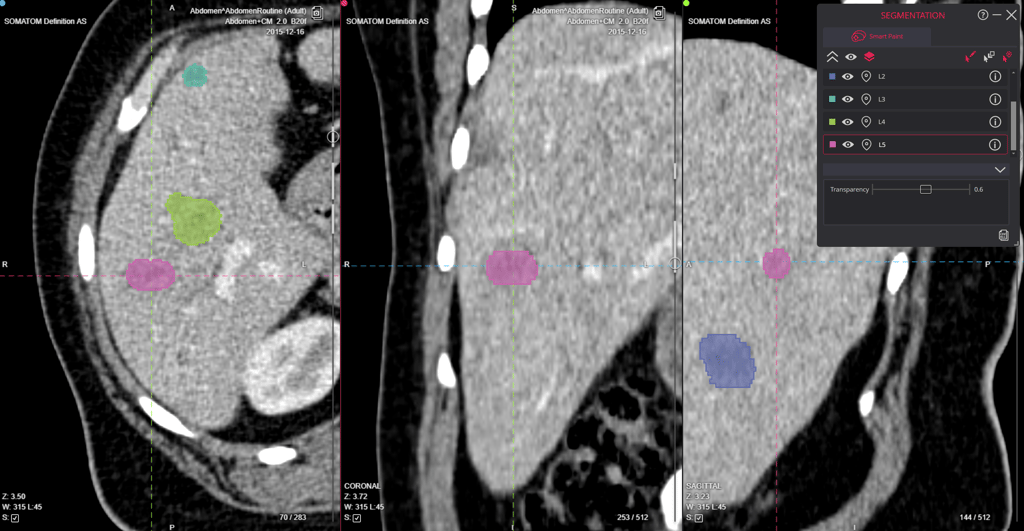
5. Image Analysis and Interpretation
The acquired images are analyzed using predefined methods, which may include:
- Quantitative measurements
- Visual assessment by trained readers
- Computer-aided detection or analysis
- Artificial intelligence algorithms
6. Data Analysis and Reporting
Results are compiled and analyzed to answer the study's research questions, with findings eventually published in medical journals.
Also Read: Imaging Biomarkers: Complete Guide to Medical Diagnostic Indicators
Virtual Imaging Trials: The Next Frontier
A fascinating development in the field is the emergence of virtual imaging trials (VITs), which use computer simulations to evaluate imaging technologies without requiring human subjects.
According to the Radiological Society of North America (RSNA):
"In radiology, imaging trials are used similarly to evaluate and optimize the design and clinical use of medical imaging devices and methods."
Virtual imaging trials offer several advantages:
- Cost and Time Efficiency: VITs significantly reduce the time and costs associated with traditional trials.
- Flexibility: Researchers can easily vary the characteristics of virtual patients and repeat trials as needed.
- Safety: No radiation exposure or other risks to human participants.
- Diversity in Testing: VITs can capture a wide range of anatomical variations, enhancing the realism of the trials.
These simulated trials are particularly valuable for evaluating AI technologies in radiology, providing datasets with precise ground truth to assess the validity of AI claims.
Also Read: Automated Clinical Trials Medical Imaging Platform
The Role of Imaging Clinical Trial Management Systems
Managing the complex data generated in imaging trials requires specialized tools. Imaging Clinical Trial Management Systems (ICTMS) are purpose-built platforms that streamline this process.
An ICTMS is defined as:
"A specialized software platform designed to streamline the collection, analysis, and management of medical imaging data in clinical trials."
These systems offer several key features:
- Centralized image storage
- Automated workflow management
- Quality control tools
- Advanced analytics capabilities
- Regulatory compliance features
- Integration with other clinical trial systems
By implementing an ICTMS, research teams can enhance data quality, accelerate study timelines, improve collaboration, and facilitate more accurate endpoint assessments.
Benefits and Challenges of Imaging Trials
Benefits
Imaging trials offer numerous advantages for medical research and patient care:
- Non-invasive Assessment: Many imaging techniques provide valuable information without invasive procedures.
- Early Detection: Imaging can often detect disease changes before clinical symptoms appear.
- Objective Measurements: Imaging provides quantifiable data that can be analyzed statistically.
- Visualization of Disease: Researchers can directly observe disease processes and treatment effects.
- Surrogate Endpoints: Imaging findings can serve as surrogate endpoints, potentially shortening trial duration.
According to Medpace:
"Imaging technologies, such as MRI and ultrasound, come with a number of advantages, including non-invasiveness and the potential for early outcome detection."
Challenges
Despite their benefits, imaging trials face several challenges:
- Standardization: Ensuring consistent image acquisition across multiple sites and equipment.
- Interpretation Variability: Different readers may interpret images differently.
- Cost and Resources: Advanced imaging can be expensive and require specialized equipment.
- Data Management: Handling large volumes of imaging data securely and efficiently.
- Regulatory Considerations: Meeting regulatory requirements for imaging endpoints.
Prospective Multicenter Imaging Trials
Prospective multicenter imaging trials represent one of the most robust approaches to imaging research. These studies involve multiple research sites following standardized protocols to collect imaging data over time.
According to a comprehensive guide on here at Collective Minds :
"A prospective multicenter imaging study is a forward-looking research project conducted across multiple medical institutions, using standardized imaging protocols to evaluate specific clinical outcomes."
The success of these trials depends on:
- Protocol Design: Incorporating standardized imaging parameters and quality control measures.
- Data Management: Using HIPAA-compliant systems for secure data handling.
- Quality Assurance: Implementing regular equipment calibration and centralized quality control.
- Centralized Management: Utilizing platforms that integrate various aspects of trial management.
Also Read: Centralized Imaging Core Labs for Multicenter Trials
Imaging as Biomarkers in Clinical Trials
One of the most valuable applications of imaging in clinical trials is the use of imaging biomarkers—quantifiable features in medical images that can indicate biological processes, disease progression, or treatment response.
According to Keosys:
"Medical imaging is a key asset in the drug development process as it can provide efficacy evaluation and safety monitoring data needed in clinical trials."
Imaging biomarkers offer several advantages:
- They can be measured objectively and quantitatively
- They often detect changes earlier than clinical symptoms
- They provide spatial information about disease location and extent
- They can be repeated over time to monitor changes
The FDA increasingly accepts imaging biomarkers as surrogate endpoints in drug approval processes, which can significantly lower costs and expedite trials for life-threatening diseases.
FAQ: Common Questions About Imaging Trials
What is the difference between an imaging trial and a clinical trial?
While both are research studies involving human participants, imaging trials specifically focus on evaluating imaging technologies and their applications, whereas clinical trials typically test treatments, interventions, or preventive measures.
Who can participate in imaging trials?
Eligibility varies by study. Some imaging trials recruit healthy volunteers, while others seek participants with specific medical conditions. Each trial has defined inclusion and exclusion criteria.
Are imaging trials safe?
Most imaging procedures used in trials are considered safe, though some involve radiation exposure or contrast agents that carry minimal risks. All potential risks are explained during the informed consent process.
How long do imaging trials last?
The duration varies widely depending on the study objectives. Some imaging trials involve a single imaging session, while others may require multiple sessions over months or years.
How can I find an imaging trial to participate in?
You can search for imaging trials on ClinicalTrials.gov, ask your healthcare provider, or contact academic medical centers and research institutions in your area.
What is an imaging exam for?
According to Johns Hopkins Medicine: "Imaging tests are common tools used by health care providers to screen for medical problems, diagnose diseases and conditions, monitor existing conditions, and assess whether treatments are effective."
Conclusion
Imaging trials play a vital role in advancing medical science and improving patient care. By systematically evaluating imaging technologies and their applications, these specialized research studies help develop better ways to detect, diagnose, and monitor diseases.
From traditional approaches to cutting-edge virtual trials, the field continues to evolve, offering new opportunities to enhance our understanding of disease processes and treatment effects. As imaging technologies advance, so too will the methods used to evaluate them, ultimately benefiting patients through more accurate diagnosis and personalized treatment approaches.
Whether you're a healthcare professional, researcher, or potential trial participant, understanding the fundamentals of imaging trials provides valuable insight into this important aspect of medical research.
Reviewed by: Carlos Santín Carballo on May 28, 2025