Imaging Endpoints for Medical Device Approvals: FDA Guidelines & Best Practices

In medical device development, imaging endpoints serve as critical components for regulatory approval. These specialized metrics derived from medical imaging provide objective evidence of a device's safety and efficacy, playing a pivotal role in the FDA's evaluation process. For manufacturers navigating the path to market, understanding how to properly implement and validate imaging endpoints can mean the difference between approval success and costly delays.
What Are Imaging Endpoints and Why Are They Important for Medical Device Approvals?
Imaging endpoints are quantifiable measurements or assessments derived from medical images that serve as objective indicators of a medical device's performance or a patient's response to treatment. These endpoints provide visual evidence that can be measured, standardized, and reproduced—qualities that make them particularly valuable in the regulatory approval process.
For medical device manufacturers, properly designed imaging endpoints offer significant advantages in the approval pathway. They provide objective, quantifiable data about device performance that can demonstrate treatment effects which might not be apparent through other clinical assessments. When validated appropriately, imaging endpoints often serve as surrogate endpoints, potentially shortening the time needed for clinical trials while helping satisfy the FDA's requirement for substantial evidence of safety and effectiveness.
According to the FDA's guidance on Clinical Trial Imaging Endpoint Process Standards, Imaging can provide information about the safety and effectiveness of a medical product that is difficult or impossible to obtain by other methods. This underscores the unique value imaging brings to the regulatory process.

FDA Requirements for Imaging Endpoints in Medical Device Trials
The FDA has established comprehensive guidelines for the use of imaging endpoints in clinical trials supporting medical device approvals. These requirements focus on ensuring the reliability, reproducibility, and clinical relevance of imaging data across four key areas.
Imaging Acquisition Standards
Proper image acquisition forms the foundation of reliable imaging endpoints. The FDA guidance emphasizes the importance of standardization across all aspects of image capture. This includes implementing consistent imaging protocols across all trial sites to ensure uniformity in the data collected. Patient positioning and preparation must follow standardized procedures, with appropriate timing of image acquisition relative to device use clearly defined in the protocol.
Quality control procedures are essential to ensure image consistency throughout the trial. This includes regular calibration and maintenance of imaging equipment to maintain performance standards. As noted in the FDA's guidance document, "Standardization of image acquisition across clinical sites is essential for reducing variability in the imaging outcome measures."
Display Standards
How images are displayed for review can significantly impact interpretation and ultimately affect trial outcomes. The FDA requires consistent display parameters including brightness, contrast, and resolution settings across all review stations. Appropriate viewing conditions must be established and maintained, with standardized image presentation formats to ensure reviewers see images in the same way.
Calibrated viewing monitors are necessary to maintain consistency, along with thorough documentation of all display settings used during image review. These standards help minimize variability in image interpretation that could otherwise compromise the validity of trial results.
Archiving Standards
Proper archiving ensures that imaging data remains accessible and intact for regulatory review throughout the trial and beyond. The FDA expects secure storage systems with appropriate backup procedures to prevent data loss. Complete audit trails must be maintained for any changes to imaging data, ensuring transparency and data integrity.
Both raw and processed image data should be retained, with systems compliant with 21 CFR Part 11 for electronic records. Robust data recovery capabilities must be in place to address any technical issues that might arise during the trial or subsequent regulatory review.
Interpretation Process Standards
Perhaps most critically, the FDA focuses on how imaging data is interpreted, as this directly impacts the conclusions drawn from the trial. Qualified readers with appropriate training and experience must perform image assessments. Blinded assessment procedures should be implemented to prevent bias, with standardized interpretation criteria clearly defined before the trial begins.
Independent review may be required for certain applications, particularly those involving subjective assessments or high-risk devices. Thorough documentation of interpretation methods is essential for regulatory review and validation of results.
Also Read: FDA Guidelines for Imaging Trials: Ensuring Quality and Safety in Clinical Research
Types of Imaging Endpoints Used in Medical Device Approvals
Different types of imaging endpoints serve various purposes in medical device trials, each with specific regulatory considerations that manufacturers must understand to design effective studies.
Anatomical Endpoints
Anatomical endpoints measure physical characteristics visible on imaging that demonstrate a device's effects or placement. These include dimensional changes such as size, volume, or area measurements that may show disease progression or treatment response. Structural integrity assessments can verify that implanted devices maintain their form and function over time.
Position or migration tracking helps ensure devices remain properly placed after implantation, while tissue response imaging around implanted devices can demonstrate biocompatibility and integration. These endpoints are particularly valuable for structural implants, prosthetics, and other devices where physical characteristics directly relate to performance.
Functional Endpoints
Functional endpoints assess how a device affects physiological processes within the body, providing insight into performance beyond what can be seen visually. Blood flow measurements can demonstrate improved circulation following vascular interventions, while tissue perfusion imaging shows whether tissues are receiving adequate blood supply after treatment.
Metabolic activity imaging can reveal changes in cellular function in response to therapeutic devices, and mechanical function assessments demonstrate how devices interact with surrounding tissues during movement or under stress. These endpoints are especially important for devices designed to restore or enhance physiological functions.
Surrogate Endpoints
Surrogate endpoints are imaging measurements that predict clinical outcomes, potentially allowing for shorter trials when the relationship between the imaging finding and clinical benefit has been established. Examples include tumor response measurements for oncology devices, plaque reduction imaging for cardiovascular interventions, and bone density assessments for orthopedic implants.
The FDA's Table of Surrogate Endpoints provides examples of accepted surrogate endpoints that have served as the basis for approval, though it primarily focuses on drug approvals rather than devices. Device manufacturers often need to validate the relationship between their proposed imaging surrogate endpoints and clinically meaningful outcomes.
Independent Review and Endpoint Adjudication
For high-risk devices or those with subjective imaging endpoints, the FDA often requires independent review of imaging data to ensure unbiased assessment of safety and efficacy.
"Independent clinical endpoint adjudication is critical to the assessment of the safety and efficacy of medical devices.
tudies are not blinded. Medical Device trials are often open labeled because the device investigated cannot be “hidden” from the investigator or the patient"
notes the Endpoint Adjudication Committee blog.
Implementing effective independent review requires careful planning and execution. An adjudication charter should be established early in the trial design process, clearly defining the scope, procedures, and decision-making processes for the review committee. Selection of qualified, independent reviewers with appropriate expertise is essential for credible assessments.
Robust blinding procedures help minimize bias, particularly important in device trials where complete blinding may be impossible. Consensus methods for resolving discrepancies between reviewers should be established before the trial begins, with thorough documentation of all review decisions to support regulatory submissions.
Also Read: Endpoint Adjudication in Clinical Trials
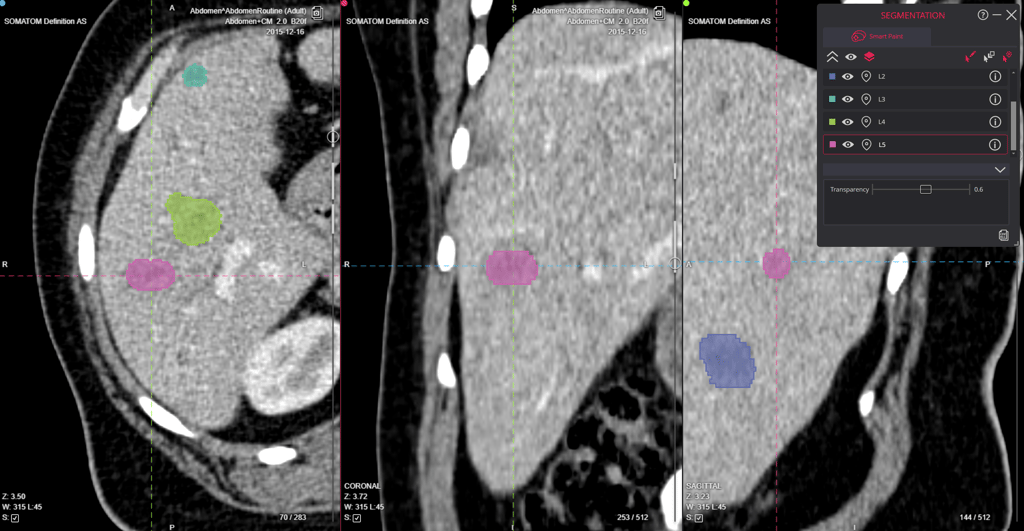
Automated Data Collection for Imaging Endpoints
Modern clinical trials increasingly rely on automated systems to collect and analyze imaging data, improving efficiency and reducing human error. These technological advances offer significant benefits while introducing new considerations for regulatory compliance.
Automation can substantially reduce variability in measurements by eliminating human inconsistency in data collection and analysis. This leads to faster data processing, enabling more efficient trial execution and potentially earlier insights into device performance. Real-time quality control becomes possible, allowing issues to be identified and addressed promptly rather than discovered during later analysis.
Enhanced reproducibility of results strengthens the scientific validity of findings, while improved audit trails support regulatory requirements for data integrity and transparency. According to imaging experts, "Automation minimizes human error and variability, accelerates data gathering and analysis, and allows for real-time monitoring, ultimately optimizing trial outcomes while reducing costs."
Despite these advantages, automated systems must still meet FDA requirements for validation, documentation, and quality control. Manufacturers must demonstrate that automated methods produce reliable, accurate results comparable to established techniques, with appropriate controls to identify and address any system failures or anomalies.
Also Read: Imaging Data Management: Essential Strategies and Best Practices
Best Practices for Implementing Imaging Endpoints
Based on FDA guidance and industry experience, several best practices have emerged for successfully implementing imaging endpoints in medical device trials. These approaches help manufacturers navigate regulatory requirements while generating high-quality data to support approval applications.
Early Engagement with the FDA
Proactive communication with regulators can prevent costly missteps in trial design. Manufacturers should discuss imaging endpoints with the FDA during pre-submission meetings to ensure alignment with regulatory expectations. This early dialogue provides an opportunity to address potential concerns before significant resources are invested in trial execution.
The FDA's feedback can help refine endpoint selection, validation approaches, and statistical analysis plans. By establishing a collaborative relationship with regulators early in development, manufacturers can create a more efficient path to approval while reducing the risk of unexpected regulatory hurdles.
Develop a Comprehensive Imaging Charter
A well-designed imaging charter serves as the foundation for consistent, high-quality imaging throughout the trial. This document should detail imaging acquisition protocols specific to each imaging modality used, with equipment specifications that ensure compatibility across trial sites. Reader qualifications and training requirements should be clearly defined to maintain assessment quality.
Interpretation criteria must be established before the trial begins, with quality control procedures that address potential issues at each stage of the imaging process. The charter should be reviewed and approved by all stakeholders, including clinical investigators, imaging specialists, and regulatory experts.
Standardize Across Trial Sites
Consistency across multiple trial locations is essential for generating reliable imaging data. This requires implementing standardized imaging protocols with detailed procedures for each imaging modality. Comprehensive training should be provided to all sites, ensuring that technicians understand and follow protocols precisely.
Central quality control mechanisms help identify and address deviations promptly. Many trials benefit from using phantoms or calibration tools to standardize equipment performance across different machines and locations. Regular site qualification and monitoring throughout the trial helps maintain compliance with imaging standards and quickly resolve any issues that arise.
Validate Imaging Methods
Before relying on imaging endpoints for regulatory decisions, manufacturers should thoroughly validate their methods to ensure scientific validity. This includes demonstrating reproducibility through test-retest studies that quantify measurement variability under consistent conditions. Whenever possible, establishing correlation with clinical outcomes strengthens the case for using imaging as a surrogate endpoint.
Validation of measurement techniques should address accuracy, precision, and limits of detection relevant to the device's intended use. Assessment of inter-reader and intra-reader variability helps quantify the human factors in image interpretation and informs statistical analysis plans for the trial data.
Ensure Proper Blinding
Minimizing bias is crucial for generating credible evidence of device performance. Effective blinding strategies include separation of image acquisition from interpretation, preventing those who know the treatment assignment from influencing image capture or analysis. Blinding readers to treatment assignment helps ensure objective assessment of imaging endpoints.
Randomizing image review order prevents sequential bias that might occur if images are reviewed in a predictable pattern. For complex or subjective assessments, using independent core labs with demonstrated expertise in the relevant imaging modality adds credibility to the findings and strengthens regulatory submissions.
Also Read: Best Practices for Multi-Centric, Multi-Modal Clinical Trials with Imaging Endpoints
Fast Track Designation and Imaging Endpoints
For medical devices addressing serious unmet needs, the FDA's Fast Track designation can expedite the review process, potentially bringing important therapies to patients more quickly. When imaging endpoints are involved in Fast Track applications, special considerations apply to ensure that accelerated timelines don't compromise data quality.
The FDA's clinical trial imaging endpoint standards for Fast Track applications maintain the same fundamental requirements as standard applications, including standardized imaging protocols that ensure consistency across all trial sites. Reliable methods for image acquisition must be implemented with appropriate quality controls, and robust procedures for analysis and interpretation are essential to support regulatory decisions.
As noted in a recent article,
"Collaborating with experienced organizations, such as Collective Minds Research for MedTech, can provide essential support in managing imaging endpoints. CMR offers specialized services, including standardized data collection protocols and regulatory compliance support, which can enhance the likelihood of a successful Fast Track application."
Introduction to Collective Minds Research.
While Fast Track designation may accelerate review timelines, it doesn't reduce the need for scientific rigor in imaging endpoint assessment. Manufacturers should work closely with imaging experts and regulatory consultants to develop streamlined approaches that maintain data quality while taking advantage of expedited review opportunities.
Also Read: FDA Fast Track Designation: A Game-Changer for MedTech Startups
Common Challenges and Solutions in Imaging Endpoint Implementation
Despite careful planning, several challenges commonly arise when using imaging endpoints for medical device approvals. Understanding these challenges and implementing effective solutions can help manufacturers navigate the complexities of imaging-based clinical trials.
Variability Across Imaging Sites
Multi-center trials often struggle with inconsistency in imaging equipment, technician experience, and protocol adherence. To address this challenge, manufacturers should implement centralized training programs that ensure all site personnel understand imaging requirements. Site qualification processes should verify equipment compatibility and performance before patient enrollment begins.
Ongoing quality monitoring throughout the trial helps identify and address issues promptly. Many successful trials incorporate phantoms or calibration tools that provide objective measures of imaging system performance, allowing for standardization across different equipment and locations.
Reader Subjectivity
Human interpretation of images inevitably introduces some subjectivity, particularly for complex or subtle findings. Developing detailed interpretation criteria with clear definitions and examples helps reduce this variability. Reader training should include test cases that establish baseline performance and identify areas needing additional guidance.
For endpoints with significant subjective components, implementing double reading with formal adjudication for discrepancies provides an additional layer of quality control. This approach, while resource-intensive, strengthens the credibility of findings and supports regulatory submissions.
Evolving Imaging Technology
Clinical trials often span several years, during which imaging technology may advance or equipment may need replacement. Manufacturers should consult with the FDA about technology transitions during trials to ensure regulatory acceptance of any changes. When equipment changes are necessary, equivalence testing should document the comparability of results between old and new systems.
Protocol amendments may be required to address technological changes, with clear documentation of the rationale and potential impact on endpoint assessment. Maintaining some overlap between old and new technologies during transition periods can provide valuable comparative data to support regulatory review.
Data Management Complexity
Imaging generates large volumes of complex data that must be managed securely and efficiently throughout the trial. Specialized imaging data management systems designed for clinical research can maintain audit trails and ensure data integrity from acquisition through analysis. These systems should comply with 21 CFR Part 11 requirements for electronic records.
Clear data handling procedures should be established before the trial begins, with defined roles and responsibilities for each step in the process. Regular data quality checks throughout the trial help identify and address issues before they impact study outcomes.
Regulatory Uncertainty
Imaging endpoints, particularly novel approaches, may face regulatory uncertainty regarding acceptance as primary endpoints. Engaging with the FDA early and often through the pre-submission program helps align expectations about imaging endpoints and their role in demonstrating device safety and effectiveness.
Manufacturers should consider including traditional clinical endpoints alongside imaging measures, particularly for first-in-class devices or novel imaging approaches. This parallel assessment can help establish the relationship between imaging findings and clinical outcomes, strengthening the regulatory case for current and future applications.
Future Trends in Imaging Endpoints for Medical Device Approvals
The landscape of imaging endpoints continues to evolve, with several emerging trends likely to shape future regulatory approaches. Manufacturers who understand and prepare for these developments will be better positioned to leverage new opportunities in device development and approval.
Artificial Intelligence and Machine Learning
AI algorithms are increasingly being used to analyze imaging data, potentially offering greater consistency and detecting subtle patterns human readers might miss. These technologies can reduce reader variability while potentially identifying new imaging biomarkers relevant to device performance. The FDA is developing frameworks for evaluating AI-based imaging endpoints, with particular attention to validation, transparency, and performance monitoring.
As these technologies mature, manufacturers should consider how AI might enhance their imaging endpoint strategies while preparing for the regulatory considerations specific to algorithm-based assessments. Early engagement with regulators about AI approaches can help establish appropriate validation requirements and performance metrics.
Novel Imaging Modalities
Advanced imaging technologies like molecular imaging, functional MRI, and photoacoustic imaging are expanding the types of endpoints available for device evaluation. These modalities can provide insights into biological processes and device-tissue interactions not visible with conventional imaging, potentially enabling more sensitive and specific assessments of device performance.
Manufacturers exploring novel imaging modalities should invest in validation studies that establish the relationship between these advanced measures and clinically meaningful outcomes. Collaboration with academic centers and imaging experts can accelerate the development and regulatory acceptance of these approaches.
Patient-Centered Imaging Endpoints
There's growing interest in correlating imaging findings with patient-reported outcomes to ensure that imaging endpoints reflect meaningful clinical benefits. This patient-centered approach aligns with broader regulatory trends emphasizing real-world impact over surrogate measures alone. By demonstrating how imaging findings relate to symptoms, function, or quality of life, manufacturers can strengthen the clinical relevance of their endpoints.
Future trials may increasingly incorporate both imaging and patient-reported measures, with statistical approaches that explore relationships between these different assessment types. This integrated approach can provide a more comprehensive understanding of device performance from both clinical and patient perspectives.
Standardized Imaging Biomarkers
Efforts to develop and validate standardized imaging biomarkers may streamline the regulatory process by providing pre-validated endpoints for certain device categories. Industry consortia and academic collaborations are working to establish reference standards, acquisition protocols, and analysis methods for commonly used imaging measures.
These standardized approaches could reduce the validation burden for individual manufacturers while increasing consistency across trials and products. Participation in these standardization efforts can help manufacturers influence developing standards while preparing for their eventual implementation in regulatory pathways.
Conclusion
Imaging endpoints represent a powerful tool for demonstrating the safety and efficacy of medical devices in the regulatory approval process. By understanding FDA requirements, implementing best practices, and addressing common challenges, manufacturers can leverage imaging data to support successful submissions and bring innovative devices to patients more efficiently.
The key to success lies in early planning, standardization, proper validation, and ongoing quality control throughout the clinical trial process. As imaging technologies continue to advance, manufacturers who master these principles will be well-positioned to navigate the regulatory landscape efficiently and effectively.
For medical device companies seeking approval, investing in robust imaging endpoint strategies isn't just a regulatory necessity—it's a competitive advantage that can accelerate time to market and strengthen evidence of clinical benefit. By partnering with imaging experts, engaging proactively with regulators, and implementing quality-focused processes, manufacturers can optimize their use of imaging endpoints to support successful device approvals.
FAQ
What is the difference between an imaging endpoint and a clinical endpoint?
An imaging endpoint is a measurement or assessment derived from medical images, while a clinical endpoint directly measures a patient's health, function, or survival. Imaging endpoints often serve as surrogate endpoints when they're proven to predict clinical outcomes. For example, tumor shrinkage visible on imaging might serve as a surrogate for improved survival in cancer treatment devices.
Does the FDA prefer certain imaging modalities over others for medical device approvals?
The FDA doesn't generally prefer specific modalities but evaluates whether the chosen imaging method is appropriate for the specific device and indication. The key considerations are whether the imaging technology is validated for the intended measurement and whether it provides meaningful data about safety and effectiveness. The most appropriate modality depends on the device type, anatomical location, and specific endpoints being assessed.
How should we handle imaging protocol deviations during a clinical trial?
Protocol deviations should be documented, and their impact on endpoint assessment should be evaluated. Minor deviations might be addressed through sensitivity analyses, while major deviations might require exclusion of affected images from the primary analysis. A predefined plan for handling deviations should be included in the statistical analysis plan to ensure consistent, transparent decision-making throughout the trial.
Is central reading of images always required for FDA approval?
Central reading isn't always required but is strongly recommended for trials where the imaging endpoint is subjective or critical to the primary efficacy assessment. The FDA generally expects independent assessment when imaging is used for primary endpoints in pivotal trials. For objective, quantitative endpoints or secondary measures, local reading with appropriate quality control may be acceptable, though this should be discussed with regulators during trial planning.
How do we determine the appropriate sample size for an imaging endpoint?
Sample size calculations should consider the expected effect size, the variability of the imaging measurement (from pilot studies or literature), and statistical power requirements. Consulting with both imaging and statistical experts during trial design is recommended to ensure adequate power while minimizing unnecessary patient exposure. Preliminary studies to establish measurement variability can provide valuable data for more precise sample size calculations, potentially reducing overall trial size and cost.
Reviewed by: Carlos Santín Carballo on May 27, 2025