DICOM Modalities: A Comprehensive Guide to Medical Imaging Technologies
Medical imaging plays a crucial role in modern healthcare, allowing physicians to diagnose and treat patients with unprecedented accuracy. At the heart of this technological revolution lies DICOM (Digital Imaging and Communications in Medicine), the international standard for medical images and related information. In this comprehensive guide, we'll explore the various DICOM modalities, their clinical purposes, and the fascinating technologies behind them.
What is DICOM?
Before diving into specific modalities, it's essential to understand what DICOM is and why it's so important in medical imaging.
DICOM, which stands for Digital Imaging and Communications in Medicine, is the international standard for medical images and related information. According to the DICOM Standard organization
"DICOM defines the formats for medical images that can be exchanged with the data and quality necessary for clinical use."
DICOM is not just a file format; it's a comprehensive standard that includes:
- A file format definition for medical images
- A network communications protocol
- A set of services for image management, storage, and printing
This standard ensures that medical images can be exchanged, stored, and used across different systems and devices, regardless of the manufacturer.
Also Read: The Ultimate Guide to DICOM Conversion Tools: Everything You Need to Know in 2024
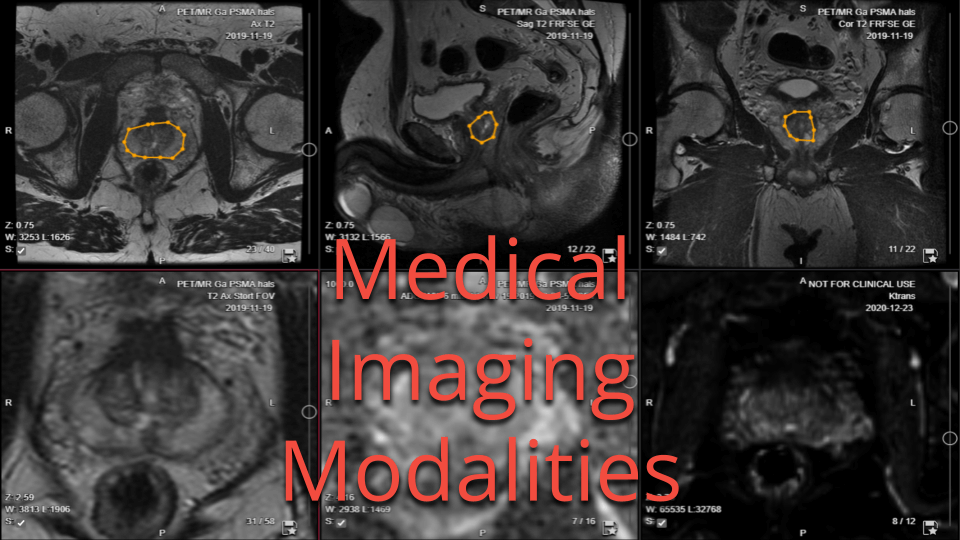
DICOM Modalities: An Overview
DICOM supports a wide range of medical imaging modalities. Each modality represents a different imaging technique, with its own unique clinical purpose and underlying technology. Let's explore the main DICOM modalities:
1. X-ray (XR)
Clinical Purpose: X-rays are used to visualize bone structures, detect fractures, and identify certain lung conditions.
How it Works: X-ray imaging uses ionizing radiation to create images of the body's internal structures. When X-rays pass through the body, they are absorbed differently by various tissues, creating a contrast that forms the image.
2. Computed Tomography (CT)
Clinical Purpose: CT scans provide detailed cross-sectional images of the body, useful for diagnosing a wide range of conditions, including cancer, cardiovascular diseases, and internal injuries.
How it Works: CT scanners use a rotating X-ray tube and digital X-ray detectors to create multiple 2D images (slices) of the body. These slices are then combined using computer processing to create detailed 3D images.
3. Magnetic Resonance Imaging (MRI)
Clinical Purpose: MRI is excellent for imaging soft tissues, making it valuable for neurological, musculoskeletal, and oncological diagnoses.
How it Works: MRI uses powerful magnets and radio waves to align hydrogen atoms in the body. When the radio waves are turned off, the atoms return to their original positions, emitting signals that are captured and transformed into detailed images.
4. Ultrasound (US)
Clinical Purpose: Ultrasound is widely used in obstetrics, cardiology, and for visualizing soft tissues and blood flow.
How it Works: Ultrasound imaging uses high-frequency sound waves to create real-time images of organs and structures inside the body. The sound waves bounce off tissues and are captured by a transducer, which converts them into images.
5. Nuclear Medicine (NM)
Clinical Purpose: Nuclear medicine is used to evaluate organ function and detect diseases at a cellular level, particularly useful in oncology, cardiology, and neurology.
How it Works: Patients are given small amounts of radioactive tracers, which accumulate in specific organs or tissues. Special cameras detect the radiation emitted by these tracers, creating images that show both the structure and function of organs.
6. Positron Emission Tomography (PET)
Clinical Purpose: PET scans are primarily used in oncology to detect cancer and monitor treatment effectiveness. They're also valuable in neurology and cardiology.
How it Works: Similar to nuclear medicine, PET uses radioactive tracers. However, PET tracers emit positrons, which produce gamma rays when they collide with electrons in the body. These gamma rays are detected to create 3D images of metabolic activity.
7. Digital Radiography (DR)
Clinical Purpose: Digital radiography is a modern form of X-ray imaging used for general radiographic exams, offering improved image quality and lower radiation doses compared to traditional film X-rays.
How it Works: DR uses digital X-ray sensors instead of photographic film. The sensors capture the X-ray image and immediately transfer it to a computer for viewing and storage.
8. Mammography (MG)
Clinical Purpose: Mammography is specifically designed for breast imaging, used both for screening and diagnostic purposes to detect breast cancer and other abnormalities.
How it Works: Mammography uses low-dose X-rays to examine breast tissue. The breast is compressed between two plates to spread the tissue and improve image quality while reducing radiation exposure.
9. Angiography (XA)
Clinical Purpose: Angiography is used to visualize blood vessels and organs, particularly useful in diagnosing and treating cardiovascular conditions.
How it Works: A contrast agent is injected into blood vessels, and X-ray images are taken to visualize the flow of blood through arteries and veins.
10. Endoscopy (ES)
Clinical Purpose: While not traditionally considered a DICOM modality, modern endoscopy systems can now output DICOM-compliant images and videos, used for examining internal organs and cavities.
How it Works: A small camera attached to a long, thin tube is inserted into the body through a natural opening or small incision. The images are captured and can be stored in DICOM format.
Also Read: What is DICOM? The Complete Guide to Medical Imaging Standards
The Importance of DICOM in Medical Imaging
DICOM plays a crucial role in modern healthcare by standardizing the way medical images are stored, transmitted, and displayed. According to a study published in a journal aboutDigital Imaging,
"DICOM has become the de facto standard for the exchange of medical images and related information."
The benefits of DICOM include:
- Interoperability: DICOM ensures that images from different modalities and manufacturers can be viewed on any DICOM-compliant system.
- Improved Workflow: By standardizing image formats and communication protocols, DICOM enhances efficiency in radiology departments and healthcare facilities.
- Enhanced Patient Care: DICOM facilitates the sharing of medical images between healthcare providers, leading to better-informed diagnoses and treatment decisions.
- Data Integration: DICOM images can be easily integrated with other healthcare information systems, such as Electronic Health Records (EHRs).
Future Trends in DICOM and Medical Imaging
As medical imaging technology continues to advance, DICOM is evolving to meet new challenges and opportunities. Some future trends include:
- AI Integration: DICOM is being adapted to support artificial intelligence applications in medical imaging, such as automated image analysis and diagnosis assistance.
- Cloud-Based Imaging: The standard is being updated to better support cloud storage and sharing of medical images.
- 3D Printing: DICOM is expanding to include support for 3D printing of medical models, which is becoming increasingly important in surgical planning and education.
-
Improved Security: As cybersecurity threats evolve, DICOM is continually updated to enhance the protection of sensitive medical data. This includes improvements in encryption, access control, and audit trails.
-
Precision Medicine: DICOM plays a crucial role in precision medicine by standardizing imaging data, making it easier to integrate with genomic and other patient data for personalized treatment plans.
-
Mobile Integration: With the increasing use of mobile devices in healthcare, DICOM is adapting to support secure viewing and sharing of medical images on smartphones and tablets.
Challenges and Limitations of DICOM
While DICOM has revolutionized medical imaging, it's not without its challenges:
-
Complexity: The DICOM standard is extensive and complex, which can make implementation and maintenance challenging for healthcare IT departments.
-
Large File Sizes: DICOM files, especially for advanced imaging modalities like CT and MRI, can be very large, posing storage and transmission challenges.
-
Privacy Concerns: As with any medical data, DICOM images contain sensitive patient information, raising concerns about data protection and compliance with regulations like HIPAA.
-
Versioning Issues: As the DICOM standard evolves, older systems may struggle to keep up with newer versions, potentially leading to compatibility issues.
-
Learning Curve: Healthcare professionals and IT staff need specialized training to fully understand and utilize DICOM effectively.
DICOM vs. PACS: Understanding the Difference
While DICOM and PACS (Picture Archiving and Communication System) are often mentioned together in medical imaging discussions, they serve different purposes:
- DICOM is the standard for formatting and transferring medical images and associated data.
- PACS is a system for storing, retrieving, and distributing medical images across a healthcare organization.
In essence, PACS uses DICOM to manage and distribute images. While DICOM ensures that images are formatted correctly and can be exchanged between different systems, PACS provides the infrastructure for storing and accessing these images within a healthcare setting.
Viewing DICOM Images
One of the advantages of DICOM is that images can be viewed on regular computers with specialized software. There are several DICOM viewers available, both commercial and open-source. Some popular options include:
- OsiriX (for Mac)
- RadiAnt (for Windows)
- MicroDicom (for Windows)
- Horos (open-source, for Mac)
- ImageJ (open-source, cross-platform)
- Collective Minds Radiology (online, free for healthcare professionals)
These viewers allow healthcare professionals to access and analyze DICOM images outside of specialized workstations, improving flexibility and efficiency in medical image interpretation. Collective Minds Radiology, in particular, offers a web-based platform that enables secure, collaborative viewing and analysis of medical images, making it an excellent resource for telemedicine and remote consultations.
The Role of DICOM in Telemedicine
The COVID-19 pandemic has accelerated the adoption of telemedicine, and DICOM plays a crucial role in this shift. By providing a standardized format for medical images, DICOM enables:
-
Remote Consultations: Specialists can review images from anywhere, facilitating expert opinions without the need for in-person visits.
-
Teleradiology: Radiologists can interpret images from remote locations, improving access to expert readings for rural or underserved areas.
-
Patient Engagement: Patients can more easily access and understand their own medical images, promoting better engagement in their healthcare.
DICOM and Artificial Intelligence
The integration of Artificial Intelligence (AI) with DICOM is one of the most exciting developments in medical imaging. AI algorithms can analyze DICOM images to:
-
Detect Abnormalities: AI can assist in identifying potential issues in images, serving as a "second set of eyes" for radiologists.
-
Prioritize Worklists: By pre-analyzing images, AI can help prioritize cases that need immediate attention.
-
Quantitative Analysis: AI can perform precise measurements and quantitative analysis of medical images, aiding in diagnosis and treatment planning.
-
Predictive Modeling: By analyzing large datasets of DICOM images, AI can help predict disease progression and treatment outcomes.
Conclusion
DICOM has become an indispensable part of modern healthcare, standardizing the way medical images are captured, stored, and shared. From X-rays to advanced 3D imaging techniques, DICOM modalities provide healthcare professionals with powerful tools to diagnose and treat a wide range of conditions.
As technology continues to advance, DICOM will evolve to meet new challenges and opportunities in medical imaging. Whether it's integrating with AI, supporting telemedicine, or enabling precision medicine, DICOM will remain at the forefront of healthcare innovation.
For healthcare professionals, IT specialists, and anyone involved in medical imaging, a deep understanding of DICOM and its various modalities is essential. By leveraging the power of DICOM, we can continue to improve patient care, enhance diagnostic accuracy, and drive the future of healthcare forward.
FAQs
-
Q: Can DICOM images be viewed on regular computers? A: Yes, DICOM images can be viewed on regular computers using specialized DICOM viewer software, many of which are freely available.
-
Q: Is DICOM only used for radiology? A: While DICOM is most commonly associated with radiology, it's used across various medical specialties, including cardiology, dentistry, ophthalmology, and pathology.
-
Q: How is patient privacy protected in DICOM files? A: DICOM includes features for data anonymization and encryption. Additionally, healthcare providers must implement proper security measures to protect DICOM data in compliance with regulations like HIPAA.
-
Q: Can DICOM files be shared via email? A: While technically possible, sharing DICOM files via email is generally not recommended due to file size limitations and security concerns. Secure, HIPAA-compliant file sharing services are preferred.
-
Q: How often is the DICOM standard updated? A: The DICOM standard is continuously evolving. Major updates are typically released annually, with minor updates and corrections published more frequently.
Appendix: Comprehensive List of DICOM Modalities
This list is based on the DICOM Standard 2024a, which is the most recent version as of the creation of this article. The DICOM standard is continuously updated, so it's always best to check the official DICOM website for the most up-to-date information.
-
AR (Autorefraction): Automated measurement of eye refraction.
-
AU (Audio): Audio recordings, such as heart sounds or dictation.
-
BDUS (Bone Densitometry (ultrasound)): Ultrasound-based measurement of bone density.
-
BI (Biomagnetic imaging): Measurement of magnetic fields produced by electrical activity in organs.
-
BMD (Bone Densitometry (X-Ray)): X-ray based measurement of bone density.
-
CR (Computed Radiography): Digital X-ray imaging using phosphor plates instead of film.
-
CT (Computed Tomography): 3D X-ray imaging using computer-processed combinations of many X-ray measurements taken from different angles.
-
DG (Diaphanography): Transillumination technique for breast imaging.
-
DOC (Document): Generic document storage.
-
DX (Digital Radiography): Direct digital capture of X-ray images.
-
ECG (Electrocardiography): Recording of the electrical activity of the heart.
-
EPS (Cardiac Electrophysiology): Waveform data from cardiac electrophysiology procedures.
-
ES (Endoscopy): Imaging of internal organs using a long, thin tube with a camera attached.
-
FID (Fiducial): Markers used for image registration and fusion.
-
GM (General Microscopy): Microscopic imaging for pathology or other laboratory examinations.
-
HC (Hard Copy): For hardcopy devices like printers and film scanners.
-
HD (Hemodynamic Waveform): Waveform data related to hemodynamic measurements.
-
IO (Intra-oral Radiography): X-ray imaging of teeth and supporting structures of the jaw.
-
IVOCT (Intravascular Optical Coherence Tomography): High-resolution intravascular imaging using light.
-
IVUS (Intravascular Ultrasound): Ultrasound imaging from within blood vessels.
-
KER (Keratometry): Measurement of the curvature of the cornea.
-
LEN (Lensometry): Measurement of the refractive power of a lens.
-
LS (Laser Surface Scan): 3D surface scanning using laser technology.
-
MG (Mammography): Specialized X-ray imaging for breast examination.
-
MR (Magnetic Resonance): Imaging technique that uses strong magnetic fields and radio waves to generate detailed anatomical images.
-
NM (Nuclear Medicine): Imaging that uses small amounts of radioactive materials to diagnose or treat various diseases.
-
OAM (Ophthalmic Axial Measurements): Measurements of the eye's axial length.
-
OCT (Optical Coherence Tomography): High-resolution imaging using light waves.
-
OP (Ophthalmic Photography): Imaging of the eye and related structures.
-
OPM (Ophthalmic Mapping): Mapping of ophthalmic features.
-
OPT (Ophthalmic Tomography): Tomographic imaging of the eye.
-
OPV (Ophthalmic Visual Field): Measurement of the visual field.
-
OSS (Optical Surface Scanner): 3D scanning of body surfaces using optical technology.
-
OT (Other): Modality used when the imaging type doesn't fit into other defined categories.
-
PLAN (Plan): For radiotherapy plans.
-
PX (Panoramic X-Ray): Wide-view X-ray of the mouth area.
-
PT (Positron Emission Tomography (PET)): Functional imaging technique using radioactive tracers to observe metabolic processes.
-
RF (Radio Fluoroscopy): Real-time X-ray imaging used to visualize internal structures in motion.
-
RG (Radiographic imaging (conventional film/screen)): Traditional film-based X-ray imaging.
-
RTIMAGE (RT Image): Radiotherapy images.
-
RTDOSE (RT Dose): Radiotherapy dose data.
-
RTSTRUCT (RT Structure Set): Radiotherapy structure sets.
-
RTPLAN (RT Plan): Radiotherapy treatment plans.
-
RTRECORD (RT Treatment Record): Radiotherapy treatment records.
-
SEG (Segmentation): Segmented data from images.
-
SM (Slide Microscopy): Digital capture of microscopic slides.
-
SMR (Stereometric Relationship): Measurement of stereometric relationships.
-
SR (Structured Reporting): Structured documents that contain text with links to other data.
-
SRF (Subjective Refraction): Subjective measurement of eye refraction.
-
STAIN (Automated Slide Stainer): For devices that automatically apply stains to microscopy slides.
-
TG (Thermography): Imaging that detects heat patterns on the skin.
-
US (Ultrasound): Imaging using high-frequency sound waves to visualize internal body structures.
-
VA (Visual Acuity): Measurement of visual acuity.
-
XA (X-ray Angiography): Imaging of blood vessels using X-rays with contrast agents.
-
XC (External-camera Photography): General photography for medical documentation.
This list represents the modalities defined in the current (at the time of writing) DICOM Standard 2024a. It's important to note that the DICOM standard is regularly updated, and new modalities may be added or existing ones modified in future versions. Always refer to the most recent DICOM standard for the most up-to-date and accurate information.
Reviewed by: Mathias Engström on October 30, 2024




